Introduction
Acute myeloid leukemia (AML) is the most prevalent acute leukemia in adults and originates from hematopoietic precursor cells that suffers genetics and epigenetics alterations leading to a clone able to proliferate with survival advantages. The last years have been of great advances in AML because of more profound knowledge of its pathogenic mechanisms. This lead to a better stratification of the patients based on cytogenetics and molecular criteria and development of targeted therapy that changed its natural course. Unfortunately, the tests and new drugs are expensive and not easily available worldwide, especially in low and middle-income countries (LMIC) with distinct realities between private and public care.
Methods
To determine the profile and outcomes of patients in a public health center in Brazil, we did a retrospective analysis of all the cases of non-promyelocytic AML diagnosed between 2007 and 2017 in the University Hospital Professor Edgar Santos of Federal University of Bahia. 62 patients were included and we used a modified model of European LeukemiaNet 2017 classification to risk stratification, with cases of secondary AML (sAML) included in the high risk group.
Results
A total of 62 patients were analyzed, 1 died prior treatment and was excluded. Median age at diagnosis was 44 years (range, 16-83 years) with 58% females. 68% werede novoAML. 11% of patients were classified as favorable risk, 8% as intermediate and 42% as high risk. 39% had unknown risk because of absence of cytogenetic and/or molecular tests.
The chemotherapy protocol in patients eligible to intensive treatment was 7+3 in 87%. 20% of the patients died during induction and 65% achieved response (53% complete + 12% partial remission). Analyzing only sAML, 35% were considered fit for intensive treatment and most of less intensive regimens were based in low-dose cytarabine (64%). The overall response rate of sAML after induction was 20%.
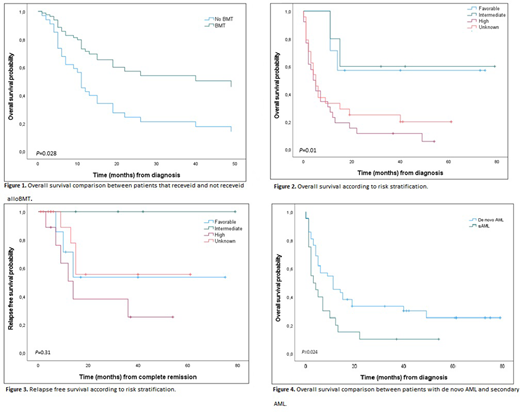
During the treatment, 31% relapsed with a median time to relapse of 8 months. 43% of the relapses happened in patients classified as unknown risk. 37% of patients that survived induction were submitted to allogeneic bone marrow transplant (alloBMT) and had survival advantage (hazard ratio, HR: 2,52, 95% CI: 1.103 - 5,795;P= 0.028; Figure 1), with superior median overall survival (mOS) (49 months) when compared with the chemotherapy group (11 months) (P= 0.021).
During the follow-up, 77% of the patients died and most of the deaths (61%) occurred in the first year of diagnosis. The primary cause of death was infection (52%) followed by leukemia progression (31%). The mOS was 7 months and 5-year OS was 27%. Stratifying by the risk, the mOS was shorter in patients with unknown and high risk (5 and 4 months, respectively) than in low and intermediate risk (not reached,P= 0.01; Figure 2). The median relapse free survival (RFS) was 15 months, reached only in the high risk group (14 months;P= 0.31; Figure 3). The patients with sAML had mOS of 3 months versus 11 months ofde novoAML(P =0.024; Figure 4).
Discussion
In summary, we found statistical difference in better OS among patients that received BMT, AMLde novoand favorable/intermediate risk. Our findings were similar to those reported by other groups of university hospitals in Brazil.
An alarming data is the high proportion of patients who were not adequately stratified. Our data are from real life and this subgroup still exists because cytogenetic and molecular tests are not universally available in the brazilian public health system. Those patients had similar outcomes to high risk ones suggesting that a proportion of them were undertreated. It is important for every center to be aware of their survival curves to better individualize their approaches. We suggest that patients with inadequate risk assessment should undergo alloBMT as this remains the primary curative intervention and the main outcome changer in real-world setting of LMIC.
Our high mortality rate, in comparison with data from developed countries, reflects the absence of more effective therapies, especially for high risk cases, and an inferior hospital infrastructure contributing to a higher incidence of infections. Considering the discovery of new powerful drugs, the tendency of discrepant outcomes between centers from LMIC and developed countries is considerably high. Therefore, the improvement of access to diagnostic techniques and treatment is still an unmet need in AML scenario.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal